This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing.
This issue focuses on Dr. Rola Ajjawi.
Dr. Ajjawi is Scientist at CHES and Professor in the Department of Surgery. She sees this role being about developing educational research capabilities and generating new knowledge about medical education practice and research for UBC and the field broadly. More importantly it’s about supporting colleagues new and old in the field to find their niche and what inspires them. Her research is broadly about how to enrich workplace learning.

How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
By mistake mostly, although I come from a family of educators, my dad was a professor of adult education, my mother and sister are high school teachers, so perhaps it was inevitable. After becoming a physiotherapist, and early in my career, I took up a clinical educator position – facilitating student learning of cardiopulmonary physiotherapy in the medical and surgical wards as well as intensive care. I was interested in the physiology of treatment and preventing comorbidities for patients for best quality of life. But I quickly realised that I didn’t really know much about education or how best to support student learning in the clinical environment. That led to a PhD in health professions education and then my first job in medical education at the University of Sydney.
What was your first research project about?
My first research project was my honours thesis during undergrad – it was a three dimensional biomechanical analysis of the hip, knee and ankle during lateral stepping exercise. I know … numbers right! At that time it took a whole day to synthesize the biomechanics at these joints for one participant. It was cool technology though, right at the start of using the 3 markers on each segment to calculate limb movement. It feels a lifetime ago. It’s probably still the most quantitative study I have ever done! Today I enjoy the freedom and richness that comes with in-depth qualitative research and no spreadsheet in sight.
What have you been exploring in your current scholarship?
My interests are diverse, I’m still dabbling in feedback particularly interested in enabling productive feedback cultures and purposefully decentering the supervisor as the main source of feedback information. Understanding belonging, especially for marginalised students, and the moments that matter to students during their university studies is another thread. And finally, making assessment and digital practices more equitable in and through education.
What is the most important lesson you have learned from doing education research?
It never goes according to plan – and that’s ok. Good research generates more questions. Getting the research question right is fundamental (most of the time). Being open and flexible to emergent ideas, theories, data, participants is important, following where the research leads. Good research takes time, having good people around you whose judgement you trust and who you enjoy working with makes the best research. Ok so that’s more than one lesson!
What HPE research finding or theory has had the greatest impact on your work?
Learning about sociocultural theories when doing my PhD really expanded my perspective on what education could be and do. Understanding the agency / structure debate helped me to appreciate why changing practice is so hard. More recently, engaging with sociomaterial theories and the new materialists has been intellectually fun but finding ways to apply it in the day to day, more challenging.
 What would you describe as your most significant contribution to HPE scholarship so far?
What would you describe as your most significant contribution to HPE scholarship so far?
Broadening the unit of analysis beyond the individual when thinking about workbased learning, feedback, assessment, etc. I guess my most significant contribution has been asking: what else is going on here?
What do you like to do outside of work?
I like being outdoors (in the sun preferably) with my dog hiking, swimming, kayaking, eating, hanging out with friends. Exploring new places and cultures is always fun. Going to anything live from sport to music to theatre and art. I’m new to Vancouver and Canada – so lots to try including pickleball.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing.
This issue focuses on Gaby Yang.
Gaby Yang is a Pediatric Intensivist at Victoria General Hospital in Victoria, BC, and Clinical Assistant Professor in the Department of Pediatrics. She completed the Master of Health Professions Education Canada Program through CHES in 2022. Presently much of her non-clinical time is dedicated to the MD Undergraduate Program where she is the Course Director for MEDD 421 and the Written Exam Pillar Lead with the Provincial Learner Assessment Team (PLAT).

 What or who inspired you to make teaching and/or education such a prominent part of your career?
What or who inspired you to make teaching and/or education such a prominent part of your career?
All the residents and attending physicians who contributed to my learning as a medical student. These individuals taught me how to think as a clinician and helped me build a firm foundation for my clinical practice. It was their ability and generosity to guide me that has made me the clinician that I am today. Having experienced firsthand the difference a skilled educator can make in one’s training, I want to be able to ‘pay it forward’. I hope I’m also able to impart what I have learned and help the next generation of medical trainees transition to competent clinicians.
What is your favorite part of the educational process? What keeps you inspired?
Seeing the ‘aha’ moment in a trainee when the myriad of foundational knowledge they’ve amassed come together clinically. During each education encounter, I seek to identify the gaps in the learners’ understanding and then help them narrow that gap by scaffolding their existing knowledge to strengthen their clinical reasoning framework. Recognizing that adult learners have a range of learning style and needs, I love the challenge of finding new ways of presenting information to clarify concepts for learners. It inspires me to think broadly about curricular design and how to provide the right feedback to support learning.
What has been the most important lesson you have learned through your teaching and innovation?
Dare to try. While there is wisdom in using instructional methods that have been tried and true, as educators we need to also be open to trying new ways of thinking and learning. Learning can occur through so many ways. What has worked for learners in the past may no longer be as relevant to our future learners. As someone who enjoys the comfort of certainty, this is a lesson I’m continually learning.

What is one practical tip you might share with new faculty members who wish to pursue education as a prominent part of their career path?
There are more opportunities than there is time. So, no need to rush into anything. Take your time, connect with the Med Ed community to become acquainted with the scholarship that is happening locally, and then commit to opportunities that align with your interests in the education process.
What do you like to do outside work?
Nowadays I’m appreciating a life of slowness. Taking time to smell the flowers and rediscovering the joy of reading fiction. But when I can, I love to escape to somewhere warm and explore the underwater world!
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on James Tessaro. James Tessaro is a General Internist at St. Paul’s Hospital in Vancouver, BC. He is the Program Director for the UBC General Internal Medicine (PGY4/5) Postgraduate Training Program. He completed his CHES Clinical Educator Fellowship at UBC and Masters of Health Professions Education at Maastricht University.


How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
My involvement in research in health professions education started slowly. Like many who have had the privilege to train in the UBC Internal Medicine residency program, I was inspired by my preceptors who combined exceptional patient care with exceptional teaching. Some of those preceptors for me were Drs. Steve Wong, Barry Kassen and Stephane Voyer. The goal was to become a great internist and also a great teacher. Soon enough the goal of becoming a great teacher led down the slippery slope of doing research in health professions education.
What was your first research project about?
My first research project with Drs. Rose Hatala and David Shanks was about learning the procedural skill lumbar puncture. At least that’s what I thought it was about. It turned out to be more about the concept of metacognition. Before this project, I hadn’t really considered that you could think about your own thinking and that this could modify your performance. This first foray into the medical education research piqued my interest and led me to apply for the CHES Clinical Educator Fellowship.

What have you been exploring in your current scholarship?
After my clinical educator fellowship, I complete the Quality Improvement Program (Cohort 6) through the Fraser Health Authority. Now, in my role as Program Director for the UBC General Internal Medicine (GIM) Fellowship training program, with my excellent team, we are trying to systematically apply a quality improvement lens to the various elements of teaching and learning within the GIM program. We’ve been able to successfully build, analyse and improve new training experiences like incorporating telephone advice into training. We look forward to launching a new initiative to gather patient feedback on fellow performance.
What is your favorite part of the educational process? What keeps you inspired?
My favourite part remains the bedside learning. It might be something as small like having a trainee newly detect and understand a particular physical exam finding after helping them adjust their examining technique. It’s rewarding to be a part of medical trainees gaining exercise and moving along their trajectory of learning.
What is one practical tip you might share with new faculty members who wish to pursue education as a prominent part of their career path?
Find a mentor. And tell that person that you see them as a mentor.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Tristen Gilchrist. Tristen is a Clinical Assistant Professor in the Division of General Internal Medicine. For the core Internal Medicine residency program, he is the Associate Program Director responsible for curriculum. He also serves on the Competence Committee for the GIM Fellowship Program. At Vancouver General Hospital, he is Medical Co-Director of the Internal Medicine Clinical Teaching Unit, which is also his primary clinical worksite.

 How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
I stumbled into research through my interests in teaching and health education leadership. It seemed like a way to answer questions and challenges that I saw, and I was encouraged by my amazing mentor Rose Hatala to try asking a research question. And then later, research was a required component of my masters so I was stuck with it! Then my supervisor, Andrea Gingerich, convinced me to apply for a grant as a way of motivating myself to complete my masters research proposal – only for me to be awarded the grant and have a larger project than I might otherwise have taken on. I still think Andrea tricked me.
What was your first research project about?
The first one for which I took the lead was exploring how Internal Medicine academic half days were different across residency programs in Canada. Rose is probably still disappointed that I never actually wrote it up or disseminated the work in any way!
What have you been exploring in your current scholarship?
In an extension of my masters work, I’ve continued to work with Rose and Andrea exploring the dyadic supervision relationship between attendings and senior residents on the clinical teaching unit. Currently, we are focusing on indirect supervision and help-seeking and how “checking-in” behaviours relate to these. I’m also collaborating on a multi-institution study examining how EPAs connect to learning cues and conditions in residency training.
What is the most important lesson you have learned from doing education research?
Do projects with people you like to work with! Whether it’s going well or you’re coming up against challenges, it’s all more fun and manageable if you’re doing it with the right people.
What is your favorite part of the educational process? What keeps you inspired?
I still really get a kick out of seeing “a-ha” moments in my learners. Watching someone turn the corner and understand something that they didn’t before, and knowing that you helped them get there – I love it every single time. 
What is one practical tip you might share with new faculty members who wish to pursue education as a prominent part of their career path?
Find good mentorship. Look for people who have careers you think you’d like, and start talking to them. I could not have accomplished any of the things I have without having people I trust and admire giving me advice along the way.
What do you like to do outside of work?
Number one is travel. I have been to 33 countries across North America, Asia, Europe, and Africa. I still need to get to Oceania, South America, and maybe even Antarctica some day! I also enjoy being out on my bike, going for a run, visiting breweries with my partner and our dog, downhill and cross-country skiing, watching good (and bad) TV with our friends, reading, cooking…
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Saleem Razack. Dr. Razack is first and foremost a Pediatric Intensive Care physician at BC Children’s Hospital. He always says that first because, for him, everything comes from his experiences as an educator of fellows, residents, advanced practice nurses, and medical students in the PICU. By “everything”, Dr. Razack means the research questions, mostly in equity and anti-racism, which have driven his research program in health professions education. Dr. Razack is appointed as a professor of pediatrics within the Department of Pediatrics at UBC and as a Scholar at the Centre for Health Education Scholarship.

How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
In many ways, I exemplify the community of practice idea of movement from “legitimate peripheral participation” to “full participation” in medical education scholarship and research. When I began my practice in PICU, I saw myself as a teacher, rather than as an educator. There were very few role models, and educational interests were seen as secondary to more traditional biomedical research, so I would not have known that there was such a thing as an educator focused upon the pedagogy of medical or health professions education. All this changed when I attended a faculty development workshop at McGill, where I was for 25 years, on giving effective feedback to residents. I started to see that there might be a right way and a wrong way to engage in these educational actions, and that they could be studied. Plus, I found that there was a community of practice of many like minded individuals (FAC DEV devotees as I refer to them!) who saw the wonder in watching learners grasp new concepts and become trained professionals. Slowly I was drawn into the world of educational program leadership (first as a residency program director). I still count being a residency program director as the best job I ever had – 20 years later, I can look at the successes of the people I was fortunate to have in the program I was given the privilege to be the director of, and engage in a little avuncular pride for their accomplishments! In educational program leadership, the program was the generator of many research questions with respect to residency education, and I was again drawn into the world of educational research.
What have you been exploring in your current scholarship?
My focus has always been on building more equitable health care through attention to what is being taught, modelled and learned with respect to equity, diversity, inclusion, and anti-racism – in short how does social justice intersect with pedagogies of health professions education and how ought it to? Currently, I am exploring the knowledge systems of medicine itself – what we teach and how we teach it – with respect to white supremacy, patriarchy, cis- and hetero- normativity, and ableism and how this came to be. Just prior to this interrogation, I was focusing on professional socialization with respect to these issues, but for me, the key point is that the very knowledge we teach – in journal club, when we misspeak and refer to “race” as the risk factor in some disease or the other, versus referring to “being racialized as" or “experiencing racism as” as the true risk factor, or in the infectious diseases lecture where we only learn about being Gay when we learn about HIV, to give two examples—is imbued with power that includes the privileged and excludes the structurally marginalized.
What is the most important lesson you have learned from doing education research?
It is a journey where you encounter many friends, some of whom see the world or the phenomenon you are interested in through very different glasses than you do. And it is ok! Collaborate with them. Talk. Argue. Grow in your own understandings. I liken the field of health professions research to an agora of ideas. In this agora there are apples on sale with kumquats, mangoes, and occasionally partridgeberries from Newfoundland! By this I mean that one might access epidemiological methods, or critical discourse analysis, or ethnography, just to name a few, in order to apprehend the phenomenon of interest.
What HPE research finding or theory has had the greatest impact on your work?
Without a doubt, it has been critical discourse analysis. I have a huge confession: 20 years ago, I was googling people like Michel Foucault, Pierre Bourdieu, and Mikhail Bakhtin. Foucault, for me, was “that French power guy”. But I dug in; I read; and allowed my mind to expand into new ways of knowing. I am in particular, very fond, of the work of Mikhail Bakhtin. His theories of language fit so well with the complex multi-voiced phenomena that we study today in health professions education. By complex and multi-voiced, I mean domains of study such as “competence” or “professionalism”, or “equity”.
What would you describe as your most significant contribution to HPE scholarship so far?
I was fortunate with colleagues to obtain a SSHRC grant to undertake a discourse analysis of the student selection process for entry into medicine. This is where I whet my appetite for critical discourse analysis. This was the first of its kind and occurred during a time where we were seeing studies that quantified disparities in medical classes in relation to the social demographics of society—so “what” kinds of questions—but no “why is it occurring” kinds of questions. The greatest epiphany for me was to understand that the majority of “why” questions speak to the motivation of agents who participate in a particular phenomenon (e.g. “the selection of students for medicine”) and need to be studied through lenses of knowledge-power relationships. One of the synthesis papers that resulted from this study is probably among my most cited.
What is your favorite part of the educational process? What keeps you inspired?
My favourite part of the educational process is watching people acquire expertise and clinical comfort – so this would be learning in day to day care of patients. My absolute favourite part of the process is to watch over two years how PICU fellows become intensivists. Our relationship is very close – through phone calls, discussing consults etc. I am given the privilege to glimpse into the minds and thought processes of these remarkable individuals. This inspires me and gives me a sense of great privilege.
What do you like to do outside of work?
I have 5 year old twins, and I am barely coping! We are two older Dads, and the physicality of it all is mindboggling! Seriously, they take up a lot of time and energy. So spending time with them is a key activity. For myself, I am an avid reader and cyclist, and I love to cook!
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Laura Yvonne Bulk. Dr. Bulk is an Assistant Professor of Teaching in Occupational Science and Occupational Therapy. She is the Academic Lead for the Fraser Valley cohort, which accepts its first students in August 2023. Laura is a daughter, sister, tante (that means auntie, and it’s new!), a friend, mentor, mentee, learner, teacher, JEDI activist, Disabled scholar, occupational therapist, artist. She is a Dutch settler and is privileged to belong among, be in relationship with, and engage in meaningful occupations on the unceded, ancestral, and continually occupied territories of the xʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh Úxwumixw (Squamish), Tsleil-Waututh (Slay-wa-tuth), and W̱SÁNEĆ (Saanich) Peoples.

How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
I sort of fell into research generally and HPE research specifically. I just wanted to be an Occupational Therapist. As a first-generation university student from a farming family (flower farming anyway), I had no idea what all of academia might hold in terms of research opportunities. My first, albeit brief, introduction to research was a course in my bachelor of anti-oppressive social work practice at the University of Victoria. What stands out from that course is learning about participatory approaches to research. During the first months of my Master of Occupational Therapy program at UBC, I was invited to be part of the steering committee for a project with Dr. Tal Jarus and Michael Lee from the department. They were part of a newly formed international consortium focused on access for Disabled folks in HPE, known as the Inclusive Campus project at UBC. The rest is a long story, but that was the start! And I was hooked.
What was your first research project about?
For my first research project I co-designed a workshop about Disability disclosure in HPE and practice. We conducted qualitative and quantitative evaluations to understand the impacts of the workshop and to explore the nuances of disclosure for HPE students.
What have you been exploring in your current scholarship?
 I am blessed to be part of several teams, and to have my finger in many pies so-to-speak. For the past several years, I have been particularly enamoured with the concept of belonging (and non-belonging). I notice it everywhere! I’ve just started a project with two other OT faculty members (one in Prince George, one in Vancouver) and two MOT students – we are exploring processes of belonging specifically in the context of a distributed program. I am also involved in the D’HoPE (Diversifying Health Professions Education) project. This is an interprofessional project involving staff, students, and faculty from 7 HPE programs at UBC. We have designed a summer program introducing secondary and undergraduate students from equity-denied groups to HPE programs, admissions processes, and all the hidden knowledge to which they might not be privy (much of which I was not as a young adult). I also continue my collaborative and interprofessional work exploring Disability access and JEDI (Justice, Equity, Diversity, Inclusion) more broadly in HPE and practice through the ongoing inclusive campus project, Alone in the Ring (research-based theatre), and collaborations with disability access professionals at the Centre for Accessibility and beyond UBC. How can we co-create teaching and learning spaces where we embrace everyone’s humanity and invite belonging for all who might choose it?
I am blessed to be part of several teams, and to have my finger in many pies so-to-speak. For the past several years, I have been particularly enamoured with the concept of belonging (and non-belonging). I notice it everywhere! I’ve just started a project with two other OT faculty members (one in Prince George, one in Vancouver) and two MOT students – we are exploring processes of belonging specifically in the context of a distributed program. I am also involved in the D’HoPE (Diversifying Health Professions Education) project. This is an interprofessional project involving staff, students, and faculty from 7 HPE programs at UBC. We have designed a summer program introducing secondary and undergraduate students from equity-denied groups to HPE programs, admissions processes, and all the hidden knowledge to which they might not be privy (much of which I was not as a young adult). I also continue my collaborative and interprofessional work exploring Disability access and JEDI (Justice, Equity, Diversity, Inclusion) more broadly in HPE and practice through the ongoing inclusive campus project, Alone in the Ring (research-based theatre), and collaborations with disability access professionals at the Centre for Accessibility and beyond UBC. How can we co-create teaching and learning spaces where we embrace everyone’s humanity and invite belonging for all who might choose it?
What or who inspired you to make teaching and/or education such a prominent part of your career? What is your favorite part of the educational process? What keeps you inspired?
This perhaps sounds cliché, but it is the relationships I get to be part of that inspired me and continue to inspire me in my teaching and research practices. For me, teaching and research are so intertwined I find it somewhat difficult to speak to one without the other. As a researcher, I learn and then share this knowledge (knowledge translation/sharing/exchange). As a teacher, I am part of a process whereby I am both sharing knowledge and perhaps constructing new knowledge with trainees/students who are my co-learners. I would not have gone down this path without the powerful relationships I experience with staff (do not forget the ‘non-academic’ staff!), students/trainees, and faculty. It is in these reciprocal relationships in which we learn and teach one another that I witness the most flourishing and that inspires me.
What idea or innovation in your teaching are you most proud of? What fun ideas or innovations are you playing with now?
I have really enjoyed playing with research-based theatre as part of my teaching practice. The Research Based Theatre Cluster got me into acting, which I hadn’t ever expected, and I quickly realized this was one of the creative teaching practices for which I’d been searching. You can experience an example in my dissertation located on UBC’s circle!
What has been the most important lesson you have learned through your teaching and innovation?
I’ve learned to speak up more readily. Sometimes I would have a question or curiosity or idea, and would not speak it aloud as it seemed to silly or obvious or, something. I am working on this.
What is one practical tip you might share with new faculty members who wish to pursue education as a prominent part of their career path? 
I’d recommend engaging with CTLT (if you’re at UBC) or a similar teaching/learning centre at your institution. From my experience, the folks there are extremely eager to fan the flame of a love of teaching and learning – and they are highly capable too.
What do you like to do outside of work?
I am well known for my love of walking – preferably with someone! And an average of 16km a day, more if I’ve got the day off. If you ever want to go walking/rolling together drop me a line! I also enjoy feeding people – baking and cooking are my relaxation time, and it is far more enjoyable when I get to share my creations. I’m also committed to working out every morning – it has become a habit over the last decade and has had a significant impact on my mental health (physical too I suppose). I’m also always game for a game (board, card, etc). I’m also trying to make time to get back into painting, perhaps starting with a mural on my door – inside, strata does not allow those sorts of shenanigans on the outside. Travelling with or to visit people I love is another joy in my life when I have the chance.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Kerry Wilbur. Kerry is an Associate Professor in the Faculty of Pharmaceutical Sciences and Executive Director of Entry-to-Practice Education. Her role involves administrative oversight of the undergraduate pharmacy curriculum and she is a supporter of the UBC Health Integrated Curriculum.

 How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
My first years in practice were spent at Vancouver General Hospital in adult general medicine. As a Clinical Teaching Unit, there was just so much clinical education going on across disciplines. It was a really stimulating learning environment for both students and professionals. As I precepted more, I became really interested in topics like best practices for performance feedback and clinical decision-making support. In 2007, I moved to Doha, Qatar as part of the country’s wave of investment in health and education. In my academic position there, I shifted into HPE research, especially the philosophical and practical aspects of how health curriculum cross geographic contexts. Chance engagement with education consultants visiting the country (Zubin Austin, University of Toronto, Cees van der Vleuten, Maastricht University) catapulted me into more formal training.
What was your first research project about?
My first ever research project was actually studying anti-Xa levels in individuals who were treated with the low molecular weight heparin drug, enoxaparin, for a clot in their lung or leg. As a pharmacy resident, I received lots of support from my pharmacist supervisor and the collaborating nurse and hematologist. My foray into education research was way less structured. I was almost entirely self-directed without real or consistent mentorship – my professional network at the time was almost entirely ‘biomedical’ in attributes and skillset! One of the faculty members in the Department of Anthropology at Qatar University was doing what I thought was a really powerful project with migrant workers using photo-ethnography. He recommended a few books and coached me through focus group data collection over coffee one afternoon!
What have you been exploring in your current scholarship?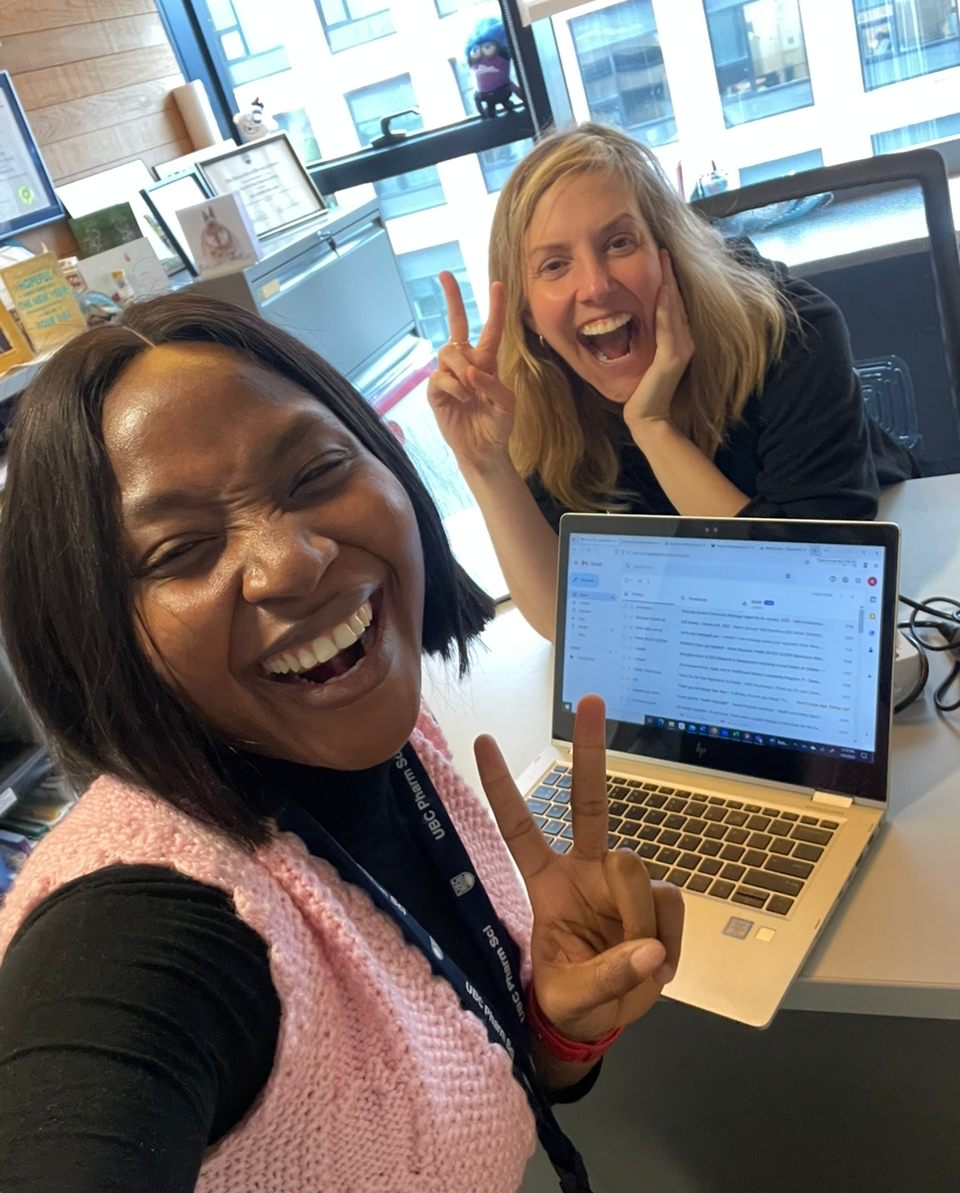
A big part of my research program is situated where my career began: in the clinical learning environment. Right now, some HPE projects I’m working on involve understanding how specific competencies, like interprofessional collaboration or advocacy, are developed and enacted by students in practice and how others assess these. Given our collective aims to train health and social care graduates to serve society, I’m also interested in how we can better enlist patients and the public in student training in meaningful ways.
What HPE research finding or theory has had the greatest impact on your work?
The use of theories in general is a revelation for someone like me trained in a health discipline! Now I love to see others apply different theories in HPE, not only from psychology or social sciences, but organizational and behavioural sciences and even further afield like economics or engineering. It’s also really satisfying when evidence and education come together – like the debunking of the myth that teaching to “learning styles” is effective. 
What is your favorite part of the educational process? What keeps you inspired?
I love the teaching teams in our Faculty. We all started off more or less as pharmacists in practice and now that we find ourselves in pharmacy education, I am inspired by their commitment to students and how they are continuously developing expertise and trying out different and imaginative ideas. Also, I could be very sad if Twitter really goes the way of the dinosaur (extinct) since the community of practice in education I have accessed there has been incredible.
What do you like to do outside of work?
I had the good fortune to travel extensively while living in Qatar and hope to resume this in some measure as Covid restrictions abate – I’m getting serious about learning Spanish! I train daily towards some sort of fitness goal (half-marathon, triathlon) and am working to redirect my volunteer time in service of things outside of the health professions; this year I am part of a group sponsoring a refugee to Canada.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Jennifer Tam. Jennifer is Clinical Assistant Professor in the Faculty of Medicine and the Pediatric Infectious Diseases Training Program Director at the University of British Columba.

How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
As my clinical fellowship in Pediatric Infectious Diseases was coming to an end in 2017, I had to decide what the right path for me was: Master of Clinical Epidemiology versus Master of Education. Most of my peers would be doing a Master of Clinical Epidemiology as this was the clear-cut choice to establish a strong foundation in clinical research, which was the mainstream route for clinicians in academic Infectious Diseases. As I sat in the office of my mentor and Program Director, Dr. Anu Wadhwa, however, she told me that the answer seemed obvious to her. Whenever I spoke about Education, I spoke with passion and excitement. Whenever I thought about Clinical Epidemiology, it seemed forced. And so, I applied for a Master of Education in Toronto (where I was doing my training at the time) and the Royal College of Physicians & Surgeons of Canada’s Robert Maudsley Fellowship for Studies in Medical Education. About two months before my fellowship was to end, however, I was abruptly offered a locum position at BC Children’s Hospital in Vancouver in Pediatric Infectious Diseases. Vancouver was home and having gone to high school across the street from BC Children’s Hospital, working there had always been my dream. Had my chance to gain advanced training in Education evaporated? Once again, Dr. Wadhwa became my sage guide and told me, “I know someone in Vancouver named Glenn who might be able to help.” This Glenn was CHES’ very own Dr. Glenn Regehr. Before I knew it, I was connected with Dr. Rose Hatala to discuss a Master of Health Professions Education (MHPE) and the Clinical Educator Fellowship Program. When I arrived in Vancouver, I was welcomed into the CHES community with open arms even though they didn’t even know me! While my path to Health Professions Education (HPE) research feels somewhat serendipitous, I couldn’t be happier with the perhaps less conventional road taken. It is hard to pinpoint exactly what drew me to this activity in the first place, but I am grateful that Dr. Wadhwa saw something that prompted her to steer me in this direction. Although I am still very new to all this HPE research, with the support that I continue to receive from the CHES community even after my MHPE, it is certainly a realm in which I intend to stay.
What was your first research project about?
My first research project in HPE was my MHPE thesis, borne out of a project idea co-developed with Drs. Anu Wadhwa and Tina Martimianakis in Toronto, and supervised by Dr. Glenn Regehr. With the rolling out of competency-based medical education and Competence Committees via the Royal College of Physicians & Surgeons of Canada, the initial idea was simply to explore a group assessment committee that had been established in one of the subspecialty training programs for the past decade that seemed to be working well. As the Royal College’s vision for Competence Committees progressively materialized, we became intrigued by a divergence that we noticed between what the members of the group assessment committee felt was most useful about the committee (i.e., the ability to speak somewhat freely about their own assessments and observations of trainees) and the Royal College’s staunch dissuasion of Competence Committees to bring anything up not already documented in a trainee’s file. As such, exploration of previously undocumented data (affectionately dubbed “PUD”) became the focus of the thesis. While we acknowledged the concerns about PUD (no one wants to be assessed by rumours or hearsay!), we found that PUD was used very responsibly by the committee and appeared to be a vital part of creating meaningful and developmentally-focused assessments beyond what documented data alone could achieve. Tam, J., Wadhwa, A., Martimianakis, M.A. et al. The role of previously undocumented data in the assessment of medical trainees in clinical competency committees. Perspect Med Educ 9, 286–293 (2020). https://doi.org/10.1007/s40037-020-00624-x
What have you been exploring in your current scholarship?
The setting of our initial exploration of “PUD” was a relatively small training program where most of the Competence Committee members would have worked closely with all trainees assessed. With the support of the Royal College’s Medical Education Research Grant, our examination of “PUD” has continued with two larger post-graduate training programs operating under the Royal College’s Competency By Design model. I am honoured to be working with Dr. Glenn Regehr again, and am also excited by the new perspectives gained working with additional incredible members of the Health Professions Education community, including Drs. Anneke van Enk, Rose Hatala, Andrea Gingerich, and Graham MacDonald! 
What or who inspired you to make teaching and/or education such a prominent part of your career?
In case it hasn’t been obvious from the previous questions, I am eternally indebted to Drs. Anu Wadhwa and Glenn Regehr for being a vital part of my involvement in Health Professions Education research.
What is your favorite part of the educational process? What keeps you inspired?
After three decades of being a student myself, I have come to appreciate that I have a relatively short attention span and simple mind. As such, I find delight in experimenting with teaching in different ways to see what makes knowledge “stick” for learners by trying to maintain learners’ attentions and simplifying concepts. I still haven’t found a magic bullet, and remain disheartened whenever I realize my “brilliant” teaching goes unretained, but I still find it fun to keep trying. What keeps me inspired is when the learning does somehow stick. So far, some of my favourites have been informal interactive half-hour whiteboard teaching with my Pediatric Infectious Diseases trainees that I call “Monday Musings”, case-based discussions, and Jeopardy!
What is one practical tip you might share with new faculty members who wish to pursue education as a prominent part of their career path?
I cannot overstate how impressed I am by the community that is CHES. If it feels like I have been doing a lot of “name dropping” in the above questions, it is because I sincerely believe that it is the people in CHES that make it such an invaluable asset to Health Professions Education. So, my one practical tip that I would tell new faculty members who wish to pursue education as a prominent part of their career path is to connect with CHES! While it can be quite intimidating being mentored by such Medical Education giants, the inclusive vibe that CHES sustains is really something special. I have sure learned a lot!
What do you like to do outside of work?
My favourite hobby is playing taiko drums, which are Japanese drums played in a group ensemble. They are usually very large drums that you hit with large sticks called “bachi”, so a great form of stress relief. It is also my main form of exercise since I am not what anyone would call athletic. I also love to travel and my bucket list is to visit every single continent – I just have Australia left! Lastly and most importantly, I find immense joy and entertainment in my 2-year-old daughter, Kayla (who is 6-months-old in the picture), and by the time you are reading this, Kayla may have a little brother!
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Sean Maurice. Sean is the Assistant Dean of the Northern Medical Program and a Senior Lab Instructor in the Division of Medical Sciences at the University of Northern British Columbia.

 How did you come to be involved in community engagement work and qualitative research?
How did you come to be involved in community engagement work and qualitative research?
I was trained as a bench scientist, studying extracellular matrix remodelling. When I took a teaching focused position at UNBC I wanted to continue doing that work and I was able to negotiate bench space and start-up funds for that purpose … but I also quickly learned of how the community of the north had fought for the university, and the medical school, which got me thinking about our responsibility to the community in a way I hadn’t felt so strongly growing up in Vancouver. This led to me wanting to engage with community, and to do what I could to support and improve rural health professions education. Within my first two years at the Northern Medical Program (NMP) I started two projects which continue to this day in some form. At the risk of looking (being?) a bit scattered academically, I enjoy the challenge of having a few very different projects on the go, along with working outside the discipline I originally trained in. Our systems are not really set up to encourage academic generalism, but I think it has a lot of value for our post-secondary institutions, to have some folks with broad and inter-disciplinary interests. My first taste of qualitative research came from a project on trust of the medical system in Carrier Sekani First Nations in north central BC (2009). I collaborated with Sarah de Leeuw (NMP), and Travis Holyk and Warner Adam from Carrier Sekani Family Services (CSFS); and collectively they supported me in learning new ways of doing research. I also got first hand exposure to the isolation and challenges of remote First Nations communities, along with the incredible strength of community in these places (Western society could learn a lot). I also learned about racism that still exists, in a very personal way. This initial collaboration has led to a variety of different projects working with CSFS over the years since. CSFS is doing a lot of creative and important work in this region and I’ve been privileged to be part of some of it. I also began work on the Healthcare Travelling Roadshow in 2009. I quite naïvely attended a rural health workforce symposium to get a better understanding of the history and challenges that the NMP was tasked with addressing. The Roadshow was an idea that came up as something that could be done within the next year, to help with the rural health workforce. I volunteered to take the lead on it and I have remained in that role as the project has grown over time. The Roadshow did not start out as a research project, but as a community engagement and university-high school outreach project, based on what we know from research; ie. that rural youth have greater barriers to overcome in pursuing healthcare career training, but if they do complete this training, they’re more likely (than their urban counterparts) to take up practice in a rural community. That is to say it fits within the scholarship of application and the scholarship of engagement (Woollard, R.F. 2006. Caring for a Common Future: Medical Schools’ Social Accountability. Medical Education 40: 301; Boyer E. 1990. Scholarship Reconsidered: Priorities of the Professoriate. Princeton, NJ: The Carnegie Foundation for the Advancement of Teaching). More recently, I have started building research around the roadshow to better understand why it’s working so well and how it could be improved. 
How did you become involved in Health Professions Education (HPE) research?
I have really enjoyed working with local First Nations and in engaging with rural youth and interprofessional healthcare students on the Roadshow. I realized along the way that there’s a great opportunity and need to study this type of work, to improve the health of some of our most important stakeholders (our stakeholders with the least access to healthcare): our rural and Indigenous peoples. I also realized that small towns and resource tight settings are often great sources of innovation, of interdisciplinary work, and of ‘common sense’ thinking; and that innovations in these settings can help not only other rural communities, but can also serve as pilots to inform potential larger scale innovations in urban settings. One of my recent projects, in collaboration with Andrea Gingerich and colleagues, is exploring how rural practitioners navigate overlapping relationships with patients. Through this work, we are elucidating how rural practitioners, by necessity, employ more sophisticated boundary navigating techniques than an urban practitioner might need to. This work is also relevant outside of the rural context and has the potential to inform how we teach all healthcare students about boundary navigation, to better prepare them for various possible practice contexts.
What have you been exploring in your current scholarship?
Currently, I’m working on better understanding rural youth perspectives on healthcare careers; a scoping review of rural university-high school healthcare career outreach projects; building a Virtual Healthcare Roadshow resource; describing how rural physicians navigate overlapping relationships; understanding equitable teaching and learning in distributed health professions education; and describing breast epithelial cell proteoglycan secretion in the invasive phenotype. 
What or who inspired you to make teaching and/or education such a prominent part of your career?
I still remember being an undergrad student and discussing with peers how many of the brightest minds at the university, were not teaching us. And while I now have a different understanding of why researchers and teachers are not always one and the same – some outstanding researchers don’t do well at translating their knowledge to first year students, and it’s not necessarily a good use of resources for the university to have their top researchers ‘bogged down’ with teaching – I still feel that effective and engaging teaching is incredibly important to our post-secondary institutions, and to society at large; and personally I like the old fashioned idea of instructors who are also active in research, or researchers who do a lot of teaching.
What idea or innovation in your teaching are you most proud of?
I recently did a lot of work on my teaching dossier for the 3M National Teaching Fellowship. This was a challenge and an opportunity to really think about what I like about teaching, what I don’t like, and what my approach is. I came up with the metaphor of adventure to describe my approach to teaching and learning. As a learner, I am at my best when I am uncertain about a new topic, but I am motivated to learn because of intrinsic interest in the topic and/or interest in the destination; ie., completing the course, or mastering new skills or knowledge. When I’m least invested in a course (I need it to graduate), I am most susceptible to a really good hook that helps me see the relevance of the topic, and helps motivate me to learn. As a teacher, I am at my best when I am a tad nervous about the topic, and thus motivated to be well prepared; and when I’m excited to try to share an important message with my learners, and thus motivated to do everything I can to make the message salient and relevant to the diversity of learners in the room. Thus, I find teaching and learning to be adventures, where uncertainty and motivation both contribute to impactful learning. 
What has been the most important lesson you have learned through your teaching and innovation?
I’m a big fan of encouraging low stakes conversations about teaching. I think teaching is hard, even for those of us who choose to have it as a major part of what we do. You can never be an expert in teaching, which is a challenging concept if you’ve trained to be an expert in a field of science or medicine. When an environment is created to share stories, people often have stories to tell, of good moments and of challenging moments. I am working on creating more space for that sharing, because it can be both cathartic and renewing, and can help build community. 
What do you like to do outside work?
I like to be outside: climbing, hiking, camping, paddling. My partner and I have really enjoyed being able to take our three teenagers on a number of really fun wilderness adventures, on the water, in the woods, and in the mountains. My newest sport is fat biking – it allows you to mountain bike through the winter – we typically get 5-6 months of snow here in Prince George, on the traditional, ancestral, and unceded territories of the Lheidli T’enneh.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Faizal Haji. Faizal is an Assistant Professor in the Division of Neurosurgery, Department of Surgery at the University of British Columbia.
How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
It all started when I was a PGY-1 resident. I was looking for a research project and one of my mentors asked me to help design a resident microvascular skills training curriculum for a live-animal lab he was running at the hospital. I had always been interested in education, but this was the first time I was introduced to simulation research and HPE broadly. Once I started to read around the literature in the area I was hooked. Based on what I learned about the ‘best practices’ in simulation, we ended up designing a two-year spiral curriculum for our junior residents that incorporated distributed learning, expert feedback, repetitive practice and structured assessment using a modified OSATS framework. The program has been really successful and has been running as an embedded part of the training program for the last 10 years. From this I decided I wanted to study simulation in greater depth, so I decided to pursue a PhD at the University of Toronto and a Research Fellowship at The Wilson Centre.
What was your doctoral research about?
As with many budding HPE researchers, initially I was interested in very practical questions about curriculum development, design, and assessment. With the help of some great mentors (including some of the senior scientists at CHES) I ended up taking a deep dive into fundamental questions about how we design simulation training. Specifically, I explored the role that fidelity (i.e. the realism of a simulation) has on learning outcomes. There is a pervasive notion that we need “high fidelity” simulation for the training to be useful, but while there is some reasonable educational theory to support this notion much of the evidence from HPE shows the opposite – that fidelity doesn’t really seem to matter most of the time. I got interested in exploring this issue during my doctoral work and that led me to other competing theoretical perspectives, including work on cognitive load and working memory, learner engagement, and information processing. What we found was that the answer isn’t simple, and that if fidelity matters it likely interacts with the experience level of a learner, what their (and the instructor’s) learning goals are, and that learners are much more active in managing their cognitive resources than what the theoretical perspectives often cited in simulation research have captured to date.
What HPE research finding or theory has had the greatest impact on your work?
I think I am a cognitivist in most of the ways that I think about my HPE work. During my PhD I spent a lot of time thinking about cognitive psychology principles like the context similarity effect and Cognitive Load Theory (CLT), and the latter one in particular has shaped a lot of my scholarship over the years. Like all productive theory testing however, the more I worked with CLT the more interesting it became – not just for the ways in which it could explain phenomena I was seeing in my work, but more importantly in the moments where the theory failed to predict the outcome I was expecting. It's these moments where the theory ‘falls apart’ that I have come to find the most frustrating but also the most interesting. I have come to believe that by leaning into these moments to try and understand why this happens, we as HPE scholars can contribute new understanding - not only in our own field but also in the scientific disciplines that we borrow from.
What have you been exploring in your current scholarship?
I have developed a wide range of research interests in HPE. I am continuing my work on simulation instructional design, now delving into questions like “what is cognitive overload, and how do learners experience, manage, and make sense of it?” and “what is learner engagement, how is it influenced by instructional design, and in turn how does it impact learning outcomes?”. In addition, I have been working on bringing together the HPE, global health and global surgery spheres. In particular, I am interested in how we employ innovations in HPE curriculum design and assessment (e.g. CBME) to inform how we engage in healthcare capacity development in resource limited settings. Finally, as a surgeon I am increasingly interested in exploring surgical cognition and how surgeons make both clinical and educational decisions in the operating room and in the context of their everyday practice. 
What would you describe as your most significant contribution to HPE scholarship so far?
That’s a tough question to answer! I’m still early on in my research career, and I am proud of some of the theoretical work our team was able to do during my doctoral years. But I think my most significant contribution has actually been a paper I wrote with a few friends about Program Evaluation in HPE. In it, we talk about the importance of considering not just whether planned outcomes were achieved (“did it work?”), but also consider whether planned processes occurred (“how did it work?”), whether planned theory appropriately accounted for the program outcomes (“why did it work?”) and what unplanned processes, outcomes, and emergent theory (“what else happened?”) can tell us about how a program is working (or not). The paper started as an assignment for a doctoral class and has ended up being one of my most frequently referenced and utilized contributions.
What do you like to do outside of work?
I love the outdoors and the water, so whenever I get the chance I take my daughters hiking, to the lake, or to the beach. We are living in Port Moody, so it’s the perfect place to be able to do any or all of these activities – rain or shine!
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Katherine Wisener. Katherine is the Associate Director for the Office of Faculty Development and a PhD candidate in the Maastricht School of Health Professions Education.

How did you get interested in doing a PhD and what went into the decision to finally jump in?
I have noticed a recurring pattern in that I will work in a given role for a few years, and then I find myself intrigued by some phenomenon to the point that I absolutely must explore it empirically. I find that the daily demands of positions don’t always allow for room to explore, ponder, and read about things that interest us, which is one reason why considering a PhD was compelling to me. I emailed Kevin Eva one evening to pick his brain about the Maastricht PhD Program in the School of Health Professions Education and before I knew it, I was drafting my application to the program. Mentorship from Sandra Jarvis-Selinger, Renate Kahlke, Erik Driessen, and Dan Pratt also gave me the water wings that helped me take the plunge.
What was your first research project about?
My very first research project was in an undergraduate psychology course where we were tasked with applying theories of persuasion. I created two different donation request forms to a charity and randomly distributed them to my classmates. I was flabbergasted by the effectiveness of some of these marketing strategies, and the experience made me realize the power of words and framing. As an example, simply adjusting whether you suggest donation amounts in descending order (e.g. $25, $15, $5), will lead you to receive significantly higher contributions than ordering them in ascending order (e.g. $5, $15, $25) as people are always looking for cues in their environment to help inform decision making.
What have you been exploring in your current scholarship?
roadly speaking, my current research aims to support and value the clinical and classroom educators who teach medical students and residents. My current study is exploring how learners approach giving feedback to their teachers and preceptors. While there are plentiful guidelines for teachers in giving feedback, there is a lack of comparable guidance for learners. Given that my previous study found that teachers highly value feedback from their learners, I hope to help optimize ‘upward feedback’ processes, as one of the many ways to support clinicians who teach.
What is the most important lesson you have learned from doing education research?
I have come to greatly appreciate and value institutional ethics review boards. The task of completing an ethics application can be time consuming, with a lot of back and forth with reviewers in an effort to clarify every detail of your proposed project. I always knew that ethics was there to protect participants, but I’ve found that in every study I’ve done, a seemingly innocuous question leads to an emotional disclosure by someone. Whether its clinicians talking about ways in which they do or don’t feel valued, or medical students talking about ways in which they’ve tried to address teaching concerns, it is important to be prepared for these situations and to offer appropriate support. Your ethics application is a good place to map this out.
What HPE research finding or theory has had the greatest impact on your work?
An oldie but a goodie is Herzberg’s (1959) two-factor theory on motivation. When we think of building someone’s motivation, we often think of it as an individual issue. This theory highlights that you could be the most motivated person in the world, and still struggle if your environmental conditions create systematic barriers. This theory reminds us that building motivation in individuals is only half the battle; the environment must be addressed as well.
What is one practical tip you might share with new faculty members who wish to pursue education as a prominent part of their career path?
 That achievement in HPE research isn’t defined by how quickly you can plow through it, and in fact, there are benefits to taking your time. I had lofty goals when I started my PhD program, but working full-time, starting a family, losing my father, and trying to keep some semblance of a work-life balance has led me to take longer than I initially wanted to. That’s okay, and if anything has given me a more well-rounded perspective. I have a better understanding of the complexities clinicians face when teaching due to my work in faculty development. I have learned about different perspectives as a result of the relationships I’ve built. I have thicker skin because at the end of the day I have two little humans who love me unconditionally. Taking your time also gives you the benefit of seeing how the current societal and political climate may be affecting your research. So, my ‘tip’ would be to give yourself the grace and acceptance to chip away, knowing that doing so can ultimately lead to a stronger contribution to HPE research.
That achievement in HPE research isn’t defined by how quickly you can plow through it, and in fact, there are benefits to taking your time. I had lofty goals when I started my PhD program, but working full-time, starting a family, losing my father, and trying to keep some semblance of a work-life balance has led me to take longer than I initially wanted to. That’s okay, and if anything has given me a more well-rounded perspective. I have a better understanding of the complexities clinicians face when teaching due to my work in faculty development. I have learned about different perspectives as a result of the relationships I’ve built. I have thicker skin because at the end of the day I have two little humans who love me unconditionally. Taking your time also gives you the benefit of seeing how the current societal and political climate may be affecting your research. So, my ‘tip’ would be to give yourself the grace and acceptance to chip away, knowing that doing so can ultimately lead to a stronger contribution to HPE research.
What do you like to do outside of work?
Trail running! I love the feeling of running through the forest and feeling far away from the hustle and bustle. I also love spending time with my family. Our sons Davis (3.5) and Cole (1.5) are my walking hearts and I love watching them grow. Everyone I speak to with older children emphasize how precious this time is, so as hard as it is to fully appreciate that perspective when I’m covered in snot, tears and who knows what else, I always try to remain present and soak up all of the moments, even the chaotic ones.
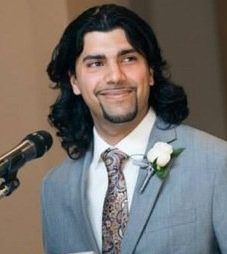
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Dr. Alasdair Nazerali-Maitland. Dr. Nazerali-Maitland is a Year 2 Clinical Skills Director for Vancouver Fraser Program, Physician Education Lead for Intensive Care ARHCC and UHNBC.

How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
Great question! I’ve always been informally involved in some sort of medical school teaching, ironically teaching clinical skills on Thursday afternoons (when post-call) while doing my Internal Medicine residency at Queen’s. From then, I had lots of questions about the how’s and why’s of things - and that led me to meet Dr. Ravi Sidhu on an elective at UBC. He was the program director for the CHES Educator Fellowship and let me sit on an Academic Half Day - and I applied to the Fellowship the next day! We had research intertwined in the Fellowship from the beginning and it was immensely helpful to navigating the matrix that is Undergraduate Medical Education.
What was your first research project about?
I was a second year IM resident – doing a project (audit) about the types of calls residents received – which, pages were able to be answered with a telephone order, a patient assessment or even just a resident-aware comment. This led us to streamlining our processes to reduce the number of low impact calls, so we could focus on urgent patient deteriorations. It was our first time presenting at ICRE.
 What have you been exploring in your current scholarship?
What have you been exploring in your current scholarship?
Clinical skills is a clinician/educator/researcher’s dream. There are so many exciting things going on and the shift between a virtual classroom setting for teaching bedside clinical examinations has been fascinating to look at. Besides expert-based policy and adaptation for COVID, we’ve been looking at clinical ultrasound teaching delivery and master teachers versus (chief) resident teachers. Sadly, my clinical work has taken me away from research for the last 18 months but our team is ready to resume this as the pandemic eases.
What is the most important lesson you have learned from doing education research?
Perhaps its my background in Critical Care which has taught me this - but the initial information (key data or background to a problem) one uses to start the foundation of any educational enquiry must be completely accurate. Take the time to do this right by really getting a lay of the land (not just starting things on a hunch), using a collaborative and wide approach of inclusivity. If this doesn’t happen, then a hypothesis is inaccurate (as the premise is ill-informed), which leads to skewed information-gathering and a conclusion which is neither relevant or reproducible. What I see time and time again (even from seasoned medical education leaders) is an inaccurate initial piece of information (or key pieces lacking) and then (unfortunately) misguided conclusions suggesting very costly and time-consuming changes which all stem from a fatal piece of misinformation.
What has been the most important lesson you have learned through your teaching and innovation?
Build a superb team and trust them to help with tasks. Paul Winwood does this extremely well and it shows. Previously in VFMP Clinical Skills, we were lucky to have a superb trio of directors that could handle the day-to-day, as well as innovate, provide concise and accurate updates to the curriculum and had practical teaching experience (two of us were CHES Fellowship alumni). We all looked forward to monthly meetings because they were so productive, collaborative and such a welcoming environment to be a part of!
What is one practical tip you might share with new faculty members who wish to pursue education as a prominent part of their career path? 
I think most of the new faculty I have met all want to take on a lot and sometimes it’s about weighing things up and politely declining some educational/career opportunities. I get some of the fellows/senior trainees to use this analogy. First, start by defining your immediate core needs (SO, children/parents, etc.) then add in absolutely necessary work/other family commitments (on call/OR slates, etc.), and then estimate what you are being asked to take on. Increase it by 10% as you want to do a good job/excel. Everyone’s substrate is different but then as the ‘stress test’ - consider how much your life could cope with, 1) an at-fault medical malpractice lawsuit, 2) illness of a first-degree family member, or 3) a significant work problem (toxic work environment, disagreement about decision-making, etc.). If that strain crosses your (personal) line of what can be handled, it sounds like the job is too much to take on at this time.
What do you like to do outside of work?
Gosh, this is a funny question these days. I’m not sure that “outside of work” exists much for an ICU doc when in the middle of a 4th pandemic wave. I love to garden and my vegetable garden was amazing this year - we had grapes, figs, blackberries, tomatoes, eggplant, kale, green peppers, lemons, lettuce and garlic. And when the time is right I like scuba-diving, travelling (Northern Japan and Marlborough, New Zealand are a couple of my go-tos), hiking, and clay-pigeon shooting.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Dr. Tandi Wilkinson. Dr. Wilkinson is a rural physician who has held a position at UBC CPD in the Rural CPD portfolio for the past ten years. In that capacity she led the development of HOUSE, an award-winning point of care ultrasound education program for rural physicians. Her research interests are the unique educational needs of rural physicians, and physician wellness. She lives in Nelson, BC and practices rural and remote emergency medicine.

 How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
In 2017 I was awarded a UBC Dept of Family Practice Rural Scholar Grant, to conduct rural research on my chosen topic of physician wellness. I quickly realized I would need mentorship to learn about research, and was fortunate to build a connection with CHES. This has been a great relationship for me – as someone who is an ‘outsider’ and new to research it was wonderful to be welcomed into the community, and to have the support needed to further my education in research.
What have you been exploring in your current scholarship?
I have just submitted to a journal my paper on informal peer support for physicians, which is a very exciting topic for me. Informal peer support has really not been studied, and yet my research showed that this form of support has been crucial to the participants in my study. Many felt they would not have been able to continue in the practice of medicine without it. If we can support access to informal peer support through medical education, we might really impact the working lives of physicians, and their patients.
What is the most important lesson you have learned from doing education research?
I was surprised to learn that even though I am new to research, I have something to offer that is in some ways unique. Most of what I have learned has been the hard way, from my lived experience. This is a great complement to an understanding of the literature, and to conducting research, and has been a real asset in my work.
What is your favorite part of the educational process? What keeps you inspired?
I love creating educational programs that are innovative and really tailored to meet the needs of learners, perhaps in new and better ways.  For instance, the ultrasound program I created offers a menu of learning options. We were the first program in Canada to ask learners what topics they needed to learn, rather than telling them what they needed to learn.
For instance, the ultrasound program I created offers a menu of learning options. We were the first program in Canada to ask learners what topics they needed to learn, rather than telling them what they needed to learn.
What has been your most memorable interaction with a class or learner?
When I taught a rural doctor and a complete beginner how to use the ultrasound machine, and the following week I got an email from that person describing how they used the ultrasound to save a patient’s life. Empowering physicians is a real joy.
What has been the most important lesson you have learned through your teaching and innovation?
It’s okay if you can’t see how to get to where you want to go. Sometimes there is no path, and you have to create your own. This is an exciting opportunity, because you can be very innovative, and perhaps create something that hasn’t been done before. It helps to stay true to what you know, to seek the input from others, and always listen to your target audience.
What do you like to do outside of work?
I like to be outside! Living rurally has allowed me wonderful access to the outdoors, and I’ve been lucky enough to do a multitude of wilderness trips throughout BC and the Canadian Arctic.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Dr. HsingChi von Bergmann. Dr. von Bergmann took on the role of Education Specialist at the UBC Faculty of Dentistry in the fall of 2010 with the responsibilities of conducting and mentoring educational research activities and designing modules and professional development activities to enhance teaching capacity and educational experiences for students in the Faculty. During the COVID-19 pandemic, she has built a virtual Learning Community for her dentistry colleagues and as a result, was nominated for the 2021 3M National Teaching Fellowship and has received two UBC teaching awards: Open Champion Award and Killam Teaching Prize. On the scholarship front, Dr. von Bergmann has received grant funding each year in the past 11 years to support her colleagues in developing education scholarship.

 How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
As a trained education researcher specialized in Science Education, I started designing research programs at the Centre for Carniofacial Molecular Biology (CCMB) at the University of Southern California (USC) in my last year of PhD study in 1997. At that time, USC was running a parallel Problem-Based Learning (PBL) pilot dental program. Although I left Los Angeles and moved to Michigan State University to continue as a senior researcher with the US-NRC Third International Mathematics and Science Study, I still remained as a research Assistant Professor with USC-CCMB, where I started the connection with Health Professions Education.
What was your first research project about?
My first research project was to understand how might PBL look like in clinical setting. I was a participant observer and tagged along with the dental students for one semester to derive at my recommendations on what PBL Clinical Dentistry can be.
What have you been exploring in your current scholarship?
Since January 2020, I have begun working with various scientists and researchers of global population health using COVID-19 data to inform and communicate pandemic mitigation directions. Also as a result of the pandemic-forced remote teaching reality, I have initiated a cross-institutional research agenda with colleagues at the University of Toronto to explore how students learn and how instructors learn to teach in online environment. A new doctoral student has been working with me on understanding professionalism in dentistry as to how students perceive it and how might professional identity can shape or enhance professionalism.
What is the most important lesson you have learned from doing education research? 
The most important lesson is that there are many interesting research ideas but too little time to enact those ideas. Prioritization of tasks is very critical to continue maintain well-being.
What do you like to do outside of work?
I enjoy outdoor activities a lot. I used to spend each summer rock climbing in the Rockies but as I am also a mother with a young child, instead of climbing, we camp and hike a lot in summer. During the pandemic, we walk a lot around the seawall and in the Pacific Spirit Provincial parks. I also run at least 5K every morning to awaken my mind to start the day.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Dr. Raheem B Kherani, Clinical Associate Professor and UBC Adult Rheumatology Program Director. Following Canadian clinical training, he completed his MHPE at Maastricht University and subsequently taught in the CHES MHPE-Canada collaboration. He provides leadership in education with a focus on postgraduate and interdisciplinary education, as well as continuing professional development (CPD). He continues to support colleagues clinically at Richmond Hospital, GF Strong Rehabilitation Centre, Vancouver General Hospital and Mary Pack Arthritis Program. As a new Program Director, he hopes to continue to foster collaboration and empowerment of his trainees and faculty. “It continues to be a privilege to serve in health care and in the education of the future leaders of tomorrow in rheumatology” says Dr. Kherani. Leading the Canadian Rheumatology Association Education Committee, coordinating the National Written Rheumatology In-Training Examination (NWRITE) and serving on the Royal College Specialty Committee are avenues to further these aspirations and facilitate ongoing engagement.

What has been the most important lesson you have learned through your teaching and innovation?
Collaboration. Through Indigenous health competency initiatives with the Canadian Rheumatology Association (CRA), I have certainly enjoyed collaboration between our Quality Care, Annual Scientific Committee and Education Committees. It has also led to developing interactive case-based role-playing to further educational opportunities in this important area of patient care for rheumatologist, rheumatology trainees and allied health. I have also seen collaboration spawn further activities at a national level within rheumatology education, with the enhancement of collaboration within the CRA Education Committee. Over the past 3 years, through restructuring the national group into the spectrum of medical education (UG, PG, CPD), we have seen a growth in activities. These have included developing a National Rheumatology Undergraduate Curriculum, providing Postgraduate CBD support, and fostering the delivery of accredited in person and virtual CPD initiatives. Connecting with CHES and the eHealth Strategy Office and rheumatology colleagues, enabled the development of video-based peer assessment to support continuing professional development. This is something that cannot happen without collaboration.
Who inspired you to make teaching and education such a prominent part of your career?
Cheryl Cox and Dr. Stephen Aaron. They both used approaches to capture my imagination and interest in pharmacy and medicine, respectively. Cheryl Cox assisted with both the development of unique pharmacy rotations, going the extra mile, to help setup rotations for a University of Alberta pharmacy student in London, Ontario and Philadelphia, Pennsylvania, as well as collaborate on Interdisciplinary Learning Initiatives between pharmacy and medicine as an early medical trainee. Dr. Aaron was engaging in case-based learning from first year medical school, which led to further clinical and research opportunities that not only spawned interest in my clinical area, but also furthered connections to develop my interest in teaching and education.
What is one practical tip you might share with trainees who wish to pursue education as a prominent part of their career path?
Engagement. Become involved in organizations within your school as well as health professional trainee organizations. This fosters collegiality, opportunities for connection, deliberation, and leadership which continue to be necessary for a future in education. These involvements continue to hone the important skill of balancing of a variety of responsibilities. 
What has been the most important lesson you have learned through your teaching and innovation?
Interactive learning. Small group learning, discussion and reflection continue to be quintessential to changing our behavior over time. Let us not just remember that it was a good session or a good speaker but strive to have a few pearls that come with it, not just for a few minutes or a few days... 
What do you like to do outside work?
Enjoyment. Contributing to my community with volunteering, biking, hiking and spending time with my family are important. They help me assist with rejuvenation and connection. I am certainly grateful for these opportunities, especially during these challenging times with the global pandemic.
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Dr. Alison Walzak, Clinical Assistant Professor at UBC, Clinical Skills Site Director of the Island Medical Program, and Director of the Clinical Teaching Unit at the Royal Jubilee Hospital.

How did you become involved in Health Professions Education (HPE) research and what drew you to this activity?
I can credit my interest in education and research to two of my earliest mentors – Drs. Irene Ma and Kevin McLaughlin. As my longitudinal Year 1 and 2 clinical skills preceptor, Dr. McLaughlin taught me many of my foundational skills, and importantly, how to treat patients with a deep sense of humanism and compassion. This has stuck with me and is something I strive to impart on my trainees. As an Internal Medicine resident, Dr. Ma helped me learn how to ask meaningful research questions and design practical programs of research, and provided the best support possible to help me become an independent researcher – the marker of a great mentor!
What was your first research project about?
My first major project involved designing a simulated night on call. I invited new PGY-1 residents to spend a 12-hour night from 8pm to 8am in the simulation lab, to give them a chance to respond to simulated ward calls. We ran only 5 cases over the night, which allowed the residents to understand what it was like to be woken up from sleep to respond to an urgent situation. The resident participants found that it decreased their anxiety in anticipation of their first real call shift, but unfortunately the human resources cost of this was quite high – it was hard to recruit senior residents to spend a night in the simulation lab to supervise!
What has been your most memorable interaction with a class or learner?
I’ve recently started to get involved in patient education through Zoom seminars. As a way to keep participants engaged, I included a few ‘dance breaks’ throughout the session. It’s pretty fantastic and inspiring to see a gallery view of patients dancing to James Brown’s “Get up offa that thing”! I’ve learned that, as a teacher, it’s important to show your learners, whether they are trainees or patients, the lighter side of medicine. 
What has been the most important lesson you have learned through your teaching and innovation?
Change is slow, but important. When I finished my training, I had grand ideas of re-vamping certain aspects of clinical teaching, and thought that it could be accomplished in a few years. Six years later, I’ve learned that evaluating the reasons for change often yields new realizations into what ought to be improved and what might be better left as-is, and that the things that fall into the former category are really worth the effort!
What is one practical tip you might share with new faculty members who wish to pursue education as a prominent part of their career path?
Try to build a team around you of mentors and peers within your career field. They are invaluable in debriefing difficult teaching encounters as they relate to your area of work, and can help build a critical mass of educational expertise.
What do you like to do outside work? 
One of my favourite ways leave work behind is to ride home – either on my bicycle or my Street Twin! My perfect day off work definitely includes a couch, a pot of tea, and a good book. When we’re not in the midst of a pandemic, I hope to get back to travelling, with Japan and Switzerland being next on my list. We’ll get there someday!
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Dr. Ingrid Price, Associate Professor of Teaching in the Faculty of Pharmaceutical Sciences at UBC.

What was your first teaching experience? How did it go?
I was a senior undergraduate student in Biological Psychology at UBC when I was given my first opportunity to teach an animal behaviour lab and – it was not good! I missed the mark in so many ways in terms of supporting student learning but through that experience I learned that I loved teaching even though I wasn’t any good at it yet. This led me to CTLT (then TAG) where I took many workshops and, eventually became a faculty developer with the unit. I have since been honoured with the Killam Teaching Prize, taught in many different environments and supported faculty members in various disciplines across campus and beyond to enhance their teaching skills. I still find teaching the most wonderful challenge – I feel as though I am always learning and improving.
What is your favorite part of teaching?
It is easily figuring out the most effective way to engage students so that they can achieve the learning objectives for whatever I am teaching. I spend a lot of time thinking about what I want students to take away from my class and how to best support them to “get there” by starting with where they are at. I absolutely love creating and implementing effective learning experiences.
What is one practical tip you would share with new teachers?
When I first started teaching, I thought that copying good teachers was what I should be doing. However, I have since learned that “one size does not fit all” with being a good teacher – there are many different types of “good” and, what works for one person may not work for another. So, try things out when you are developing your craft and be ready to let techniques go if they do not fit who you uniquely are as an instructor.
What would you say is your most significant contribution to the realm of teaching?
No longer being needed by my students! Much of my teaching in health sciences relates to the development of effective problem identification and decision-making skills. I know I have done my job when students no longer need me to help them with this process.
 Why did you enter the field of Health Professions Education (HPE) research?
Why did you enter the field of Health Professions Education (HPE) research?
My Masters and PhD are in basic science and, after being fully immersed in scientific discovery for so long part of my identity is as a scientist. While my career over the last number of years has been teaching-focused, I always knew I would to return to research. Combining research with enhancing education is the perfect partnership of my love for teaching and research. I have found that, as an educator, it can be easy to make assumptions about what is happening (and why) in a learning experience. I love that the research process requires gathering of objective data to inform my understanding ultimately allowing me to make better decisions regarding the efficacy of educational processes.
What do you most hope to accomplish through your research efforts?
I am very curious about change – how to support individuals to change as well as what holds people back from making a change. Lately, I have become interested in the role that relationship and connection can play in supporting change. Through my work in this area, I hope to develop effective ways to support faculty members and students to change and be successful in whatever they aspire to.
What do you like to do outside work?
Many things! I love being outdoors. This includes walking my beloved dog, Louis, hiking (a shot here with my sons up Hollyburn mountain on Remembrance Day a few years ago), kayaking, camping/backpacking and skiing (mostly downhill, but also cross-country). I also love sharing good food and wine with family and friends. And, over the past number of years, travelling to Europe with my husband, Willard (a shot here of us picnicking in Southern France).
This is an installment of our ‘Member Spotlight’ series, in which we feature a CHES Member and share how their area of research and innovation is impacting health professions education. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES Members may identify opportunities for collaboration and expertise sharing. This issue focuses on Dr. Brenna Lynn, Associate Dean of Continuing Professional Development (CPD) in the Faculty of Medicine at UBC.

Why did you enter the field of Health Professions Education (HPE) research?
In 2008 I was hired into the role of the Director of Continuing Professional Development (CPD) in the Faculty of Medicine. I had just finished a PhD in Cardiovascular Physiology and I was looking for a major career change – I was actively seeking something that had a great deal of impact directly on patient outcomes. It turned out to be quite the fit as there was an opportunity to start research in the field of Medical Education which I found very exciting. To be honest, I had to do a lot of reading and listening and just being curious to catch up to the field of CPD (which I had almost no experience in when I began). After I started my role, Dr. Glenn Regehr was brought to CHES as the first faculty member and we began to meet frequently to talk about research in Medical Education. This was hugely helpful in getting me more versed in the literature and what conversations were happening in the community and through this mentorship Glenn got me actively interested in the field and what contributions I could make. 
What would you describe as your most significant contribution to the field of HPE research?
Initiating a more formal CPD program of research is an accomplishment that I am proud of, and it continues to be a work in progress. Over my career, I have been actively working on bringing more of a research focus to all CPD activities whether it be through relationships, resources, or acknowledgement of the importance of this work from a leadership perspective within an academic CPD unit. Probably my biggest contribution along with the team at UBC CPD has been evolving the CPD paradigm. The field is in the midst of a major shift towards embedding learning in the workplace and alignment with quality improvement. As one of the only existing levers for change, CPD has the power to transform clinical care delivery models, support team-based practice, and close gaps in care through enhanced relationships and data-driven practice improvement. One of the main focuses of CPD is building educational programs that cultivate relationships between health professionals, for example through coaching, mentorship, or post-program support. Research shows that longitudinal, multi-exposure, and relationship-based learning is highly effective. These activities have also been shown to increase professional satisfaction and be a catalyst for meaningful and sustained practice improvement. These changes in the CPD paradigms also presents opportunities for a new research construct which we continue to explore and pursue.
What have you been exploring in your current scholarship?
As I mentioned above, our approach to CPD is very different than it used to be where traditional forms of CPD are being augmented to provide personalized and bespoke activities that aim to assist physicians and other health care professionals in successfully applying what they learn into their practices to improve the quality of patient care. I am passionate about the safe and voluntary use of data to support and influence practice improvement and CPD. The majority of health providers in British Columbia now use electronic medical records which can be a powerful tool for identifying learning needs and tracking improvements in patient care over time. Much of the scholarship has been centered on supportive relationships that health professionals build as a result of CPD interventions such as mentoring and coaching programs. I have explored perceived and unperceived needs along with barriers and enablers that promote learning in a CPD context and feel that linking CPD to QI presents and opportunity for meaningful measurement in practice.
How do you find time/structure your HPE research to ensure the work moves forward?
This presents a constant challenge in my role as Associate Dean of CPD. Scholarship and research are very important to my work and my own values but in many instances get pushed to the side of my desk due to my leadership role. In the past, I would make small attempts to keep research pursuits moving whether it was through conversation, mentorship, or writing. Recently, I have been leading a research working group within CPD to begin to formalize the thinking and doing in order to embed research into daily work so there is more structure to support in building a program of CPD research. Working with others and setting individual and group deadlines has certainly helped ensure the work continues to progress.
What do you like to do outside work?
I love running and being outdoors, anything from hiking to skiing. I have run a number of marathons including the Boston Marathon in 2011. Recently, my physical activity consists of chasing around my two young sons (Ty age 4 and Jake had his first birthday on Christmas Eve) - they both keep me on my toes. I’m looking forward to more travel with my husband and children – we have already created a bucket list of trips we want to take as a couple and as a family in the coming years.
This is an installment of our Scholar in Highlight series, in which we feature a CHES scholar and their impact in their areas of research and innovation. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES members may identify opportunities for collaboration and expertise sharing. This issue focuses on Teresa Green, an Occupational Therapist at Vancouver Coastal Health and Clinical Assistant Professor with the UBC Department of Occupational Science and Occupational Therapy.

What was your first research project about? What have you been exploring in your current research?
My first health professions education research project was the thesis project for my Masters degree in health professions education. A few years ago, I coordinated the development of a regional orientation strategy for occupational therapists hired at Vancouver Coastal Health. When we reviewed the literature to help inform the strategy, there wasn’t much there to help us. My curiosity about what is best practice for supporting new therapists led to me to explore what newly hired, new graduate OTs think of the employer supports they received when they start work. Choosing a very practical, very relevant topic kept me going even when it felt like a tough slog. Even though I have completed the degree, I am continuing on with this project. Because the prime reason for conducting this research was the lack of evidence in the literature, I would like to publish something that will hopefully be of use to other OTs. 
Current work related to education
I work as an occupational therapy clinical resource therapist at Vancouver Coastal Health. In this role, I help occupational therapists (OTs) gain the knowledge and skills they need to be able to do their jobs. My job duties include creating resources, leading education sessions and helping therapists work through clinical issues as they happen. I am also a Clinical Assistant Professor with the UBC Department of Occupational Science and Occupational Therapy. Over the years, I have done a number of roles related to occupational therapy students, including being a preceptor for fieldwork education, facilitating small group tutorials, being the clinical supervisor for student research projects and coordinating OT student fieldwork placements and clinic visits at Vancouver Coastal Health.
What is the most important lesson you have learned from doing education research?
I think the most important lesson that I have learned in my limited experience with education research is the value of having a clear plan for data analysis before collecting the data. I suppose that should be obvious, but I did need to learn it by experience.
What was your first teaching experience? How did it go?
My first teaching experience was teaching an Introduction to Rehabilitation course for rehabilitation assistant students at the College of the North Atlantic. I had only been working as an OT for a couple of years and didn’t have most of the experience the job posting asked for, but I thought ‘that sounds interesting, I’m sure I can do it’ (for not the first, nor the last time). It was a lot more work than I had expected…because it was the first year that the College offered the program, the teaching materials consisted of only a very rough outline.
What is your favorite part of the educational process?
My favourite part of the educational process is working with new graduates. I love watching them grow as therapists and seeing how relatively small actions on my part such as talking through complicated clinical cases can increase their confidence or skills and help them on their way to becoming fantastic occupational therapists providing excellent patient care.
What do you like to do outside of work?
Outside of work, my leisure activities have certainly been curtailed by working on my recently completed Masters degree. Now that I am finished, I am doing my best to catch up on my reading, baking, gardening and socializing. We have a house where friends and family often drop by for dinner. Most excitingly, I recently took up springboard and tower diving again after a decades long hiatus.
This is an installment of our Scholar in Highlight series, in which we feature a CHES scholar and their impact in their areas of research and innovation. In doing so, we hope to help propagate ideas throughout the community and provide a mechanism by which CHES members may identify opportunities for collaboration and expertise sharing. This issue focuses on Dr. Cary Cuncic, a General Internist in the Department of Medicine and a graduate of CHES' Clinical Educator Fellowship program with her Masters of Medical Education at the University of Dundee. Dr. Cuncic completed her undergraduate MD at McMaster University and completed an internal medicine residency at UBC. Dr. Cuncic's administrative roles have included Undergraduate Internal Medicine Site Lead, Associate Director of the Internal Medicine Residency Programme, and Clerkship Director for Undergraduate Internal Medicine. She is currently the Associate Curriculum Director for the MD Undergraduate Programme, focusing on years 3 and 4.

 What is your favorite part of the educational process? What keeps you inspired?
What is your favorite part of the educational process? What keeps you inspired?
My most inspiring moments in my administrative roles came from my work as Associate Programme Director of the Internal Medicine Residency Programme. For 3 years I was responsible for designing, implementing and assessing all of the remediation for 150 residents. I am amazed at the resilience of struggling learners. At times their journey seemed overwhelming, but they persevered and ended up being very successful in the programme. Reflecting on their growth and achievements continues to inspire me today. With competency by design, we are focusing on competencies rather than time, and I am hoping that we can de-stigmatize the fact that some learners simply need more time and support to achieve their competencies. I currently reserve time in my clinic specifically for struggling learners and have taken second year medical students all the way to senior residents. I act as a Remediation Supervisor and am on a team with a mission to increase the flexibility of year 3 to allow remediation time for learners who need the extra time but do not necessarily need to repeat the entire year. 
What has been your biggest challenge?
The biggest challenge I have is managing my schedule! I have competing administrative, teaching, clinical, research and personal schedules that all need to be amalgamated. For example I had to bake a cake for the school carnival “cake walk” the evening we had our big UGME retreat dinner (I baked it the weekend before and froze it … my mentor Joanna Bates has always advised me to simply buy a cake – but Joanna I could not in this case because every year I bake “the cake with the gummy bears and M&Ms”). It is inevitable that something falls apart from time to time. My goal has been to increase the intervals between those times… a work in progress. My colleagues in my division have been incredible. We all understand the complexities of the chaos of juggling and we step in to help each other all of the time. As my friend Craig says, “when you have the wrong day for a meeting, it actually doesn’t matter that you have the wrong time as well”.
What was your first research project about?
My previous research looked at a unique feedback model and we discovered that two conditions facilitated effective feedback: the teacher and learner were engaged in a longitudinal supportive relationship, and feedback was divorced from summative assessment. Building on this, I was involved in launching a coaching programme for the first year internal medicine residents: the design, the recruitment and training of coaches. Through this, we are supporting the residents to be self-regulated learners and the hope is for them to co-create learning goals with their coaches. One of my current research endeavours is to examine how this can best happen and how we can best support our coaches in this role. As Associate Director of Curriculum, I am launching a modified version of this aimed at fourth year medical students.
What do you like to do outside work? 
My personal life is hectic, noisy and busy. I have three energetic (“spirited”) boys, a dog (Newfoundlander) and a kitten. Someone is always asking me for something, someone is always hungry, someone is always running down the hall, screaming or barking. Someone always needs a bath (and no one wants to take one … well maybe the dog is OK with it). But my kids won’t be living with me forever so I focus on enjoying every minute. I like to go out with my husband and friends for good food and good wine. My husband and I like listening to jazz and will try to seek out live bands when we can. I like to read and am still in the same book club I was before I had kids. I try to stay active with my children and we ski, hike, run (my oldest and I do the Sun Run together every year) and bike.